A severe chikungunya outbreak has been reported in China with more than 7000 cases. While, chikungunya is rarely fatal, it can cause chronic symptoms like joint pain.
Chikungunya is transmitted to humans through the bite of infected mosquitoes
More than 7000 cases of chikungunya have been reported in China. Guangdong province in China is the worst-hit area, reporting the maximum number of cases. The US Centres for Disease Control and Prevention (CDC) has issued a Level 2 (Practice Enhanced Precautions) travel alert for all Americans travelling to China. The CDC has also recommended vaccination for travellers visiting an area with a chikungunya outbreak.
For the unversed, chikungunya is a viral vector-borne disease. It is transmitted to humans through the bite of infected mosquitoes, primarily the Aedes aegypti and Aedes albopictus species. The virus doesn’t spread from person to person through close contact, however, blood transmission may be possible.
What are the symptoms of chikungunya?
Chikungunya is characterised by a sudden onset of fever and severe joint pain. The incubation period is typically 3-7 days.
High fever
Severe joint pain and swelling
Muscle pain
Headache
Fatigue
Rash
Severe joint pain is one of the distinct symptoms of chikungunya, which may last for weeks, months and even years. Older adults or those with pre-existing conditions are also likely to experience severe joint pain, especially during extreme weather conditions. Other symptoms are generally self-limiting and improve within a week.
What are the treatment options for chikungunya?
Chikungunya treatment mainly focuses on relieving symptoms. Anti-inflammatory medicines and pain killers are usually used to manage fever and joint and muscle pain. Rest and adequate hydration also assist in quick recovery.
Is chikungunya fatal?
Chikungunya is rarely fatal. However, the elderly, newborns or individuals with pre-existing health conditions remain at a higher risk of severe complications.
Most symptoms are generally self-limiting and last for 2-3 days. The disease is characterised by an abrupt onset of fever, which is frequently accompanied by joint pain. Other common signs and symptoms include muscle pain, headache, nausea, fatigue and rash.
How to prevent chikungunya
Chikungunya prevention involves reducing mosquito exposure and controlling mosquito populations. Effective strategies include:
Use insect repellent containing DEET or eucalyptus oil, especially when outdoors
Wear long-sleeved clothes and full-length pants to minimise skin exposure
Use mosquito nets while sleeping, especially in areas where chikungunya is prevalent
Eliminate standing water, as this is where mosquitoes breed
Install screens on windows and doors to keep mosquitoes out
The patient’s medical background included hypertension and long-term COPD management. Her treatment plan featured enalapril for blood pressure control and a formoterol-based inhaler for her respiratory condition. For years, she had been doing relatively well.
But as her lung function began to decline, her pulmonologist decided to make an adjustment, prescribing a new combination inhaler containing indacaterol and glycopyrronium. This was considered a standard, evidence-based decision, intended to improve her breathing and slow further COPD progression.
Yet, just 48 hours after starting the new inhaler, the patient experienced something completely unexpected:
-
Painful, bright red patches appeared on her face and neck
-
She developed a mild fever
-
She reported no new cosmetics, dietary changes, or illnesses
-
She did note recent sun exposure, but with proper protection
Her sudden skin reaction and fever led to an urgent referral to dermatology.
The Diagnostic Process: Uncovering Sweet Syndrome

In dermatology, one of the greatest challenges is distinguishing between look-alike conditions. Rashes, plaques, and erythematous skin lesions can result from dozens of causes, ranging from mild allergies to serious autoimmune diseases.
The initial working diagnoses included:
-
Contact dermatitis (reaction to topical products)
-
Lupus erythematosus (autoimmune skin disorder)
-
Urticaria (hives due to allergic triggers)
However, further investigations were carried out:
-
Blood tests ruled out common infections and autoimmune markers.
-
Discontinuation of the inhaler was recommended immediately.
-
Skin biopsy was performed, and the pathology confirmed the diagnosis of Sweet syndrome.
With confirmation in hand, the patient was started on oral corticosteroids, which produced a dramatic improvement within just two days. The plaques faded, the fever subsided, and her pain diminished rapidly.
What Exactly Is Sweet Syndrome?
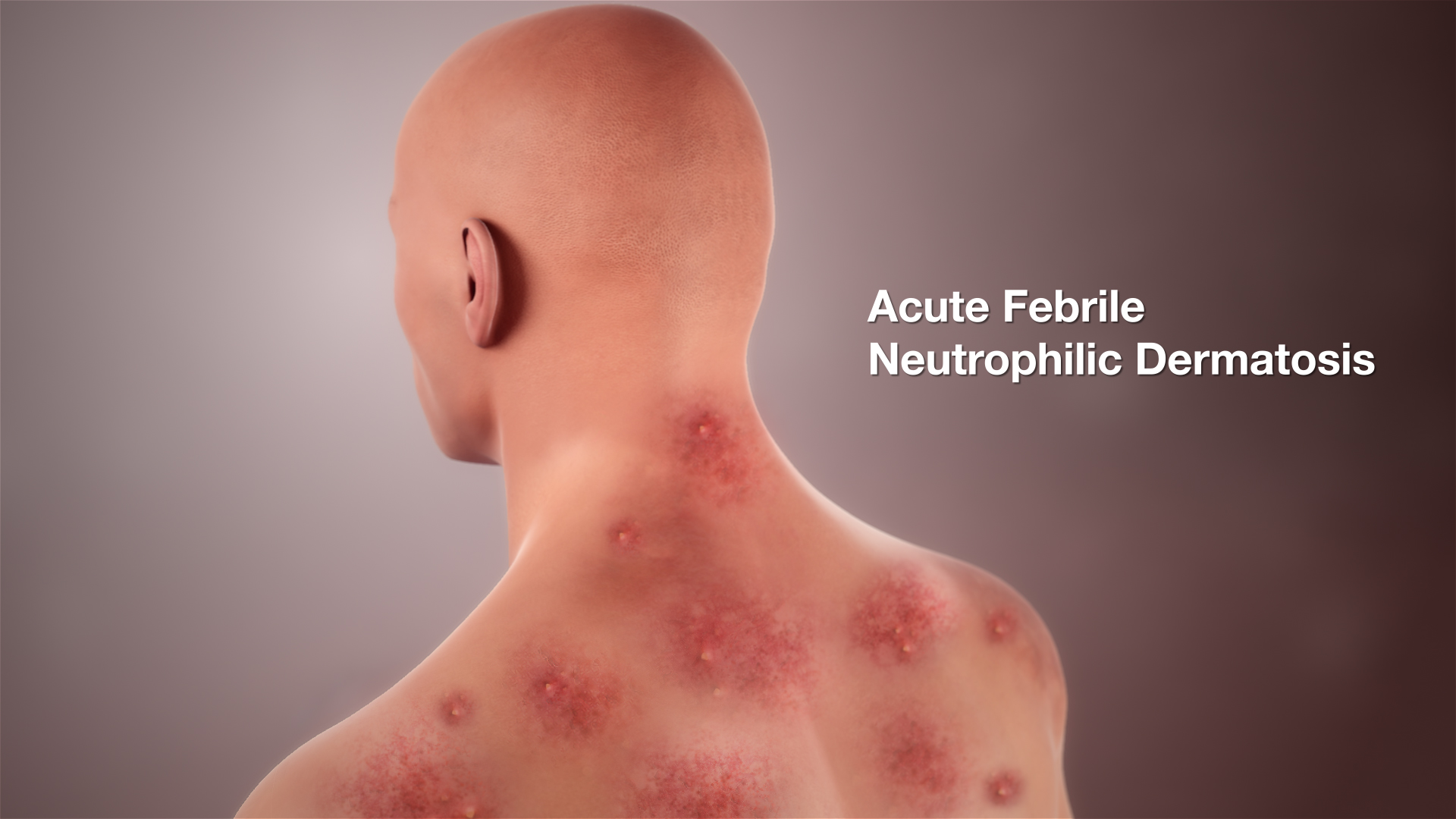
Sweet syndrome, formally known as acute febrile neutrophilic dermatosis, is a rare immune-mediated skin condition. First described in 1964 by Dr. Robert Sweet, the syndrome is characterized by:
-
Sudden onset of painful, red or purple plaques or papules
-
Lesions often concentrated on the face, neck, upper torso, and hands
-
Accompanied by systemic symptoms such as fever, fatigue, and joint pain
-
Laboratory findings often include elevated white blood cell counts, especially neutrophils
Causes and Triggers

While the exact pathophysiology is not fully understood, the condition is believed to be driven by cytokine-induced immune dysregulation, leading to neutrophilic infiltration in the skin. Known triggers include:
-
Infections: particularly respiratory or gastrointestinal
-
Hematologic malignancies: such as acute myeloid leukemia
-
Autoimmune or inflammatory disorders
-
Medications: antibiotics, antiepileptics, granulocyte colony-stimulating factor (G-CSF), and even some vaccines
Treatment usually relies on systemic corticosteroids, which often bring rapid and complete relief.
Why This Case Stands Out

The most striking aspect of this patient’s story is that her Sweet syndrome was triggered by an inhaled COPD medication. Until now, the medical literature has not reported any cases of Sweet syndrome linked to inhaled therapies.
Clinical Significance
-
Expanding the List of Known Triggers
-
Traditionally, medications associated with Sweet syndrome are oral or injectable drugs. This case suggests that even inhaled agents, which are considered safer due to localized delivery, can provoke rare immune responses.
-
-
Challenges in Diagnosis
-
Because the syndrome is rare, it can easily be misdiagnosed as more common conditions.
-
Early biopsy and recognition are crucial for rapid treatment.
-
-
The Role of Primary Care Providers
-
This case underlines how general practitioners often act as the first observers of unusual drug reactions.
-
Without quick referral and investigation, the patient’s condition could have been overlooked or mismanaged.
-
Lessons for Clinicians

For healthcare providers, this case offers important reminders:
-
Stay vigilant after medication changes
Any new drug—even those widely prescribed—can occasionally produce unexpected immune-mediated reactions. -
Consider Sweet syndrome in unusual skin eruptions
Particularly when lesions are painful, sudden, and accompanied by systemic symptoms such as fever. -
Use a broad differential diagnosis
Conditions like lupus, contact dermatitis, and drug eruptions must be excluded carefully. -
Act quickly with corticosteroid therapy
Corticosteroids remain the most effective treatment, with most patients responding within days. -
Report rare cases
Documentation helps build the medical literature, guiding future clinicians who encounter similar scenarios.
Patient Perspective: Living Through a Rare Reaction

From the patient’s viewpoint, what began as a standard inhaler change rapidly became a source of anxiety and discomfort. Painful lesions on the face and neck are not only physically distressing but also psychologically challenging, impacting self-confidence and social interactions.
Her rapid improvement with corticosteroids was reassuring, but the experience highlights the emotional burden patients face when confronted with rare and poorly understood conditions.
For patients with chronic illnesses like COPD, trust in medical treatment is vital. A rare adverse reaction can sometimes erode that trust, which is why open communication and clear explanations from healthcare providers are essential.
The Broader Implications
This case raises broader questions for both research and practice:
-
Could other inhaled therapies also carry rare immune-mediated risks?
-
Should adverse reaction monitoring systems be updated to specifically track unusual skin reactions from inhalers?
-
How can primary care doctors and dermatologists collaborate more closely to ensure rapid recognition and intervention?
Although the incidence is rare, awareness is the first step toward prevention and improved outcomes.
Conclusion: A Reminder for Vigilance
Sweet syndrome is a rare but important diagnosis that requires both clinical suspicion and rapid response. While most cases are linked to infections, cancers, or systemic medications, this unusual case demonstrates that even inhaled therapies can act as unexpected triggers.
For clinicians, the message is clear: no medication should be assumed entirely risk-free. For patients, it is equally important to report any new or unusual symptoms promptly after a treatment change.
By recognizing atypical presentations and expanding awareness of rare drug reactions, healthcare providers can ensure faster diagnoses, better outcomes, and ultimately, improved patient safety.
Sources
Stay indoors during peak hours when mosquitoes that transmit chikungunya are most active, especially at dawn and dusk.
According to the World Health Organisation, the chikungunya virus was first identified in the United Republic of Tanzania in 1952 and subsequently in other countries in Africa and Asia. Urban outbreaks were first recorded in Thailand in 1967 and in India in the 1970s. Currently, there are two chikungunya vaccines available in the United States: IXCHIQ (a live-attenuated vaccine and VIMKUNYA (a virus-like particle vaccine).